The term diffuse brain injury describes widespread brain damage. Trauma may cause diffuse axonal injury. Following trauma, secondary diffuse brain injury may occur due to oedema, haemorrhage, anoxia and infection (please note these may also occur in the context of non-traumatic brain injury).
Diffuse Axonal Injury
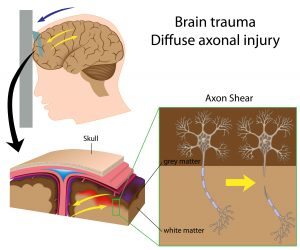 Nerve cells (neurons) consist of a cell body with an extension called an axon which connects one nerve with another. In the brain many nerve cell bodies lie near the surface making up the grey matter whilst the axons are bundled together inside and constitute the white matter. These axons carry messages to different parts of the brain and down to the brainstem and spinal cord.
Nerve cells (neurons) consist of a cell body with an extension called an axon which connects one nerve with another. In the brain many nerve cell bodies lie near the surface making up the grey matter whilst the axons are bundled together inside and constitute the white matter. These axons carry messages to different parts of the brain and down to the brainstem and spinal cord.
When the brain is subject to significant acceleration-deceleration and rotatory shearing forces (e.g. in a high speed road traffic accident, an assault, a fall), these forces can cause movement of the brain within the skull. If these forces are sufficiently strong, they will damage nerve axons resulting in diffuse axonal brain injury often extending throughout the white matter. This type of injury may not be visible on brain scanning, however it may lead to significant brain injury associated with long term disability.
Cerebral Oedema (Brain Swelling)
Swelling of the brain within the confines of the rigid skull causes raised intracranial pressure (see below), which may cause injury to the brain. Mechanisms of cerebral oedema following TBI include the following:
- Fluid may escape from blood vessels.
- The water content of brain cells may increase.
- There may be blockage of the circulation of cerebrospinal fluid (CSF) resulting in hydrocephalus.
Intracranial Pressure
Intracranial pressure (ICP) refers to the pressure inside the skull, brain tissue and cerebrospinal fluid (CSF). Normally a stable ICP is maintained by various regulatory mechanisms. ICP may vary following brain injury and if pressure is increased, this may result in further damage to brain tissue.
Raised ICP may be caused by an expanding haematoma, further haemorrhaging, development of an abscess or an increase in CSF. The skull is a rigid structure and increased accumulation of blood or CSF compresses the tissues of the brain against the skull causing further trauma to the brain and a potential reduction in the supply of oxygen leading to anoxia.
The main clinical features of raised intracranial pressure include:
- Headache, often worse in morning and aggravated by stooping or straining.
- Vomiting often without accompanying nausea.
- Papilloedema i.e. swelling of the optic disc when viewed with an ophthalmoscope.
Cerebral Ischaemia/Anoxia
Reduced blood supply to parts of the brain following TBI results in cerebral ischaemia/anoxia. Reduced blood supply occurs because of blood loss from haemorrhage and/or interference with blood circulation due to brain swelling or pressure from a haematoma. This results in brain cells not getting the oxygen they need (i.e. cerebral anoxia). This ischaemic/anoxic damage can seriously impair brain function.
Infection
In open/penetrating head injuries, where the dura is torn, a potential route for infection occurs. Bacteria can then get access to the brain and may form an abscess or may infect the meninges causing meningitis. Both require urgent antibiotic treatment and abscesses need neurosurgical drainage.