Interventions for Pressure Ulcers:
1. Follow local protocols and best practices:
• Risk assessment tools
• Wound assessment tools
• Care plans
• Grading tools
• Outcome recording
Please refer to: NHS Quality Improvement Scotland 2009, Tissue Viability Best Practise Statement ‘Prevention and Management of Pressure Ulcers’
2. It is important that staff working with people who have acquired brain injury and who are at increased risk of developing pressure sores have access to:
• Training and education
• Specialists within interdisciplinary services such as Tissue Viability team, Continence advisors and appropriate products.
• Pressure relieving equipment (e.g. air mattresses, cushion, chair) that is a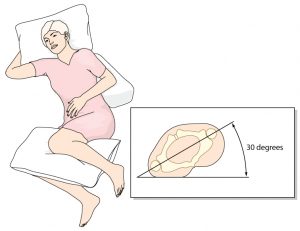 ppropriate to the individuals size and weight.
ppropriate to the individuals size and weight.
3. When working with people at increased risk of pressure ulcers, staff should:
• Implement appropriate interventions for pressure ulcers
• Regularly assess areas vulnerable to pressure, friction etc in people with mobility problems.
• Understand what factors may be contributing to the development of pressure ulcers and address these i.e. risk factors, immobility, physical impairments and continence problems.
• Encourage individuals who are able to move to do so.
• Support regular changes of position for those people who are unable to do this for themselves.
• Identify and address any issues of pain, arising either consequential to the acquired brain injury or arising from the pressure areas themselves.